In much the same way that we aren’t conscious of our lungs’ actions while breathing, we don’t exactly think about our jaws when we’re talking, having a bite to eat, or kissing a loved one. That remains true right until the moment these very normal activities cause us pain. Then, you’re suddenly extremely aware of how much we actually use our jaw and what a nightmare not being able to use it comfortably is.
The reality of the situation is that many of us will suffer from jaw pain at some point in our lives. A recent meta-analysis of temporomandibular joint (hereafter TMJ) studies shows that up to 50% of adults present symptoms of temporomandibular disorder (hereafter TMD), causing headaches, ear pain, and even degenerative bone changes in millions of people around the world (Shun Li and Leung, 2021).
Considering the risk of long-term and irreversible damage to the TMJ caused by TMD, seeking qualified and professional help in ending (or at the very least diagnosing) jaw or jaw-related pain sooner rather than later comes highly recommended.
Call 020 3865 9044 or use our portal to book an appointment at our Harley Street or Highgate clinics.
What are TMJ and TMD?
TMJ stands for temporomandibular joint, which is the hinge joint connecting the mandible (lower jaw) to the temporal bone of the skull. This joint allows our jaw to move up and down and side to side, enabling chewing, talking, and yawning.
TMD refers to temporomandibular disorder, a group of conditions that affect the normal workings of the joint, its muscles, and its surrounding tissues. TMD is sometimes also referred to as TMJD.
An easy way to understand it is that TMJ relates to TMD in the same way that ‘knee’ relates to ‘knee problems’.
What causes TMD?
TMD is typically attributed to a disorder of the TMJ; however, it can also be attributed to the masticatory muscle.
TMJ (bone and joint) causes of TMD
- Degenerative Joint Disease
- Systemic Arthritides (Inflammation of the joint)
- Condylysis/Idiopathic Condylar Resorption (Shrinkage in the ball-like end of the joint)
- Osteochondritis Dissecans (Separation of bone and cartilage)
- Osteonecrosis (Bone death due to poor blood supply)
- Neoplasm (Abnormal tissue growth)
- Synovial Chondromatosis (Growth of cartilage-like nodules)
- Fractures
- Congenital/Developmental Disorders
Masticatory muscle causes of TMD
- Myalgia (Generalised muscle pain)
- Tendonitis (Inflammation of the tendon that attaches muscle to bone)
- Myositis (Inflammation or swelling of muscles)
- Spasms
- Contracture (Tightening or shortening of muscles, tendons, or other tissues)
- Hypertrophy (Englargement of muscle)
- Systemic/Central Pain Disorders
(Schiffman and Mansur, 2016)
What are the symptoms of TMD?
Depending on the exact cause of the TMD, it could present any combination of a wide range of symptoms. While some are no more than a minor annoyance, other symptoms can cause extreme pain and discomfort and even lead to psychological effects if left untreated.
Some of the common symptoms of TMD include:
- Difficulty or pain when fully opening your mouth
- Clicking, grinding, or popping sounds when you move your jaw.
- Pain around your ear, jaw, and temple. Typically, this will present on one side of the face.
- Having your jaw lock in place when it’s open.
- Experiencing pain when chewing.
- Unexplained headaches.
(NHS, 2023)
While the list above includes the common symptoms one could expect in most TMD cases, TMD has also been conclusively linked to a range of other comorbidities, including some that you might find surprising.
Some uncommon TMD comorbidities include:
- Migraines
- Lower back pain
- Spinal pain
- Chronic fatigue syndrome
- Irritable bowel syndrome (IBS)
- Sleep disorders
- Stress
(Lee et al., 2020)
When discussing these symptoms, it’s important to understand that comorbidity doesn’t mean cause. It means that the patient has separate conditions where one might exacerbate the symptoms of another. Let’s look at the link between TMD and IBS, for example. While on the surface the two might seem completely unrelated, the stress and discomfort of dealing with chronic jaw pain could potentially trigger or worsen the symptoms of IBS, a stomach condition associated with stomach pain and bloating. In the same breath, IBS-induced stress can worsen underlying TMD as the patient unknowingly or unconsciously grinds their teeth. This also means that getting effective treatment for one of the conditions could very well lead to a lessening or reduction of the severity of the symptoms in the other.
TMD is a complex phenomenon with massive interplay between a host of other conditions. It’s important to recognise that these comorbidities are complex in nature, and if you or a loved one are suffering from TMD or even suspect that you are developing this condition, we strongly recommend seeing a physician or osteopath to get a diagnosis and discuss your treatment options. This rings especially true if you are already suffering from any of the conditions mentioned above.
How to diagnose TMD
With TMJD having such a multifactoral and complex pathology, getting a concise and accurate diagnosis of the underlying causes (and subsequently treatment options) can be a bit of a headache. Visiting your doctor complaining of jaw pain will typically result in being prescribed low-level analgesics such as paracetamol or ibuprofen, along with some basic advice such as eating soft foods like pasta or omelettes, holding an ice pack or heat pack wrapped in a tea towel to your jaw, and a demonstration on how to massage painful jaw muscles.
In more severe or ongoing cases, one might be referred to a number of potential specialists. These could include osteopaths, soft-tissue specialists who focus on the whole body and integrative, holistic approaches to diagnosis and treatment; dentists or orthodontists in the case of clear jaw misalignment; oral and maxillofacial surgeons where surgical intervention is necessary; ear, nose, and throat (ENT) specialists when the jaw pain co-presents with ear pain; rheumatologists who specialise in joint disorders; or even a neurologist, psychologist, or psychiatrists under certain conditions.
Regardless of the specialist you are referred to, they will most likely make use of MRI scans to diagnose TMD. This is the most commonly used diagnostic imaging for TMD diagnosis. Cone-beam computed tomography (CBCT) is also used to study the osseous (bone) structure for abnormalities, while ultrasound is a widely available, relatively cheap, and non-invasive method of checking for soft tissue problems (Li and Leung, 2021).
Depending on the type of specialist you are seeing, they might insist on specialised diagnostic procedures used in their field. Examples of this include bone scintigraphy, a specialised radiology procedure used to identify physical and chemical changes in bones; blood tests to check for systemic or comorbid conditions; or tissue biopsies to detect rare causes of TMD such as neoplasm (Li and Leung, 2021).
Osteopath treatment for TMD
As we’ve just learned, TMD is a complex disorder with a huge number of comorbidities. Except in select cases where there is a clear and visible cause of TMD, for example, a facial fracture or a misaligned jaw, visiting an osteopath for a diagnosis and treatment comes highly recommended.
Osteopaths focus on treating the whole person rather than just specific symptoms or illnesses. This approach is exceptionally beneficial to patients suffering from TMD, as there are so many contributing factors. A skilled osteopath will use a variety of diagnostic tools to ensure that all underlying causes and comorbidities are accurately diagnosed the first time around, leading to rapid and effective treatment. Additionally, this whole-body approach means that osteopaths often work in tandem with other specialists, ensuring that their patients get a well-rounded approach to treatment.
Stephen Sacks Osteopathy for the treatment of TMD
Stephen Sacks is a leading osteopath and has been practising in north London for over a decade. He’s registered with the General Osteopathic Council and The British Osteopathic Association and is a member of The British Medical Acupuncture Society and the International Myopain Society.
Over the years, he has helped countless people from all walks of life find relief from the misery of jaw pain. His evidence-backed and time-tested approaches to TMD treatment have repeatedly proven to be safe and effective, allowing his clients to eat normally, speak without pain, and bring smiles back to their faces.
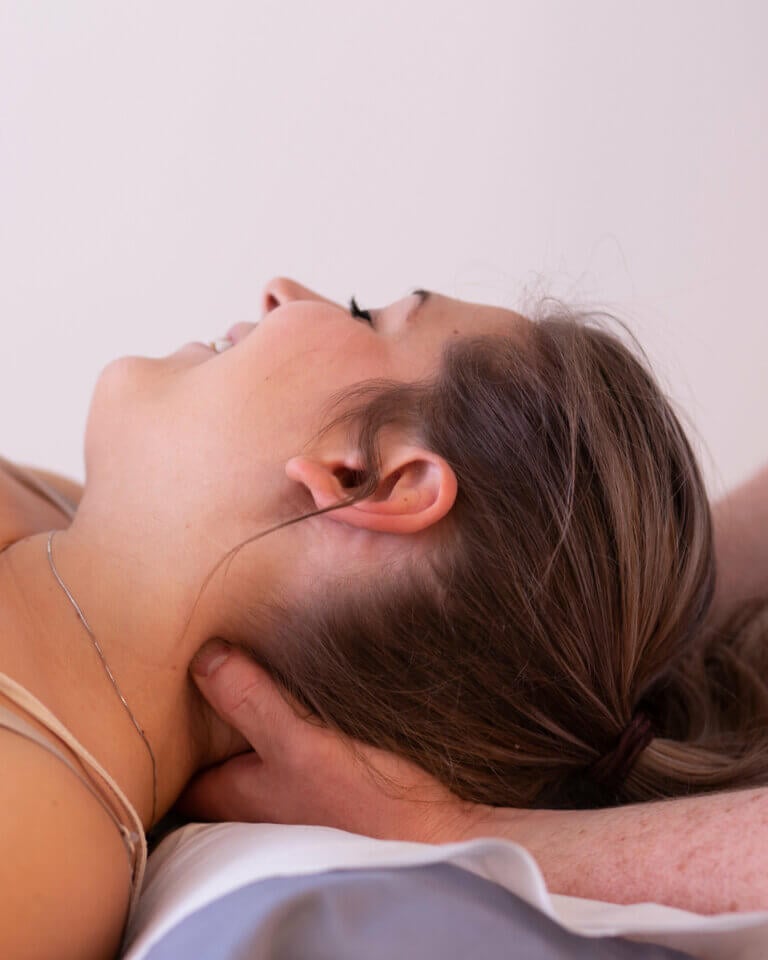
While he employs a number of techniques in the treatment of TMD, typical treatments will include soft-tissue massages, treating movement restrictions, acupuncture in specific cases, and evaluating and advising on postural causes of TMD. Depending on the severity or causes of the TMD, other techniques might applied to bring comfort.
View our Jaw Pain Service Page to learn more about how Osteopathy can be an effective treatment for TMD.
Please feel free to contact Dr. Sacks at 020 3865 9044 or through his portal for an obligation-free discussion about TMD diagnosis and treatment options.
Works Cited
Lee, KC, et al. “The prevalence of first-onset temporomandibular disorder in low back pain and associated risk factors: A nationwide population-based cohort study with a 15-year follow-up.” Medicine (Baltimore), vol. 99, no. 3, 2020. National Library of Medicine. Accessed 19 09 2023.
Li, DTS, and YY Leung. “Temporomandibular Disorders: Current Concepts and Controversies in Diagnosis and Management.” Diagnostics (Basel), vol. 6, no. 11, 2021, p. 3. National Library of Medicine, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8000442/#:~:text=While%20MRI%20is%20the%20most,34%2C35%2C36%5D. Accessed 20 09 2023.
Schiffman, E. L., and A. Mansur. “Temporomandibular Joint Disorders and Orofacial Pain.” Dental clinics of North America, vol. 60, no. 1, 2016, pp. 105-124. National Library of Medicine, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6762033/. Accessed 19 09 2023.
Shun Li, Dion Tik, and Yiu Yan Leung. “Temporomandibular Disorders: Current Concepts and Controversies in Diagnosis and Management.” Diagnostics (Basel, Switzerland), vol. 11, no. 3, 2021, p. 456. National Library of Medicine, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7220485/. Accessed 19 09 2023.
“Temporomandibular disorder.” NHS, 20 06 2023, https://www.nhs.uk/conditions/temporomandibular-disorder-tmd/. Accessed 20 09 2023.